Frailty is a condition that affects older people. UK health and social care systems need to better meet the needs of people living with frailty and their carers, especially as people with frailty are majority users for many health and social care services Improved care necessitates more robust primary care-based systems capable of routinely identifying people living with different severity grades of frailty and the application of evidence based, proactive care pathways for these populations.
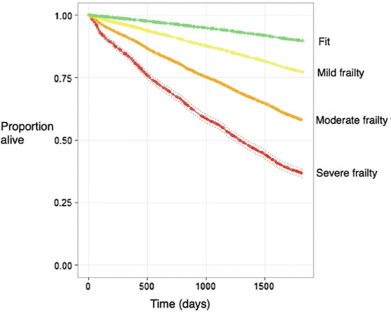
The electronic Frailty Index (eFI) is a tool which allows GPs and primary care clinicians to proactively identify and severity grade people with frailty. The eFI enables the calculation of a frailty score that can be used to identify older people with mild, moderate and severe frailty. A higher eFI score identifies older people at increased risk of care home admission, hospitalisation, and mortality. The index was developed and validated by the Academic Unit of Elderly Care & Rehabilitation, University of Leeds in partnership with TPP/SystmOne and the University of Birmingham. The eFI is modelled on the cumulative deficit model of frailty and represents a major, innovative advance in the care of older people because, for the first time, it enables identification of frailty using existing primary care data without the need for a resource-intensive clinical assessment.
Impact
GP Practices are using the eFI to understand the needs of their population, and to identify specific frailty cohorts within their practice population to offer targeted evidence based interventions toClinical Commissioning Groups (CCGs). Leading the way in terms of integrated care are using the eFI and data linkage to develop new models of care for entire populations of people living with frailty. Examples of how general practices and CCGs are using the eFI include:
- medication reviews for people with severe frailty and care home residents: NHS Vale of York CCG; NHS Harrogate & Rural Districts CCG
- proactive falls prevention interventions for people with moderate frailty: NHS Leeds South & East CCG, Birmingham Public Health Falls & Fracture Pathway
- nurse led frailty assessments for people with mild, moderate and severe frailty: NHS Hambleton, Richmondshire & Whitby CCG; NHS Scarborough & Ryedale CCG
- adding people with severe frailty to practice palliative care registers and offering advance care planning interventions: NHS Airedale, Wharfdale & Craven CCG
- identifying patients with moderate and severe frailty for comprehensive geriatric assessment clinics: NHS South Devon & Torbay CCG; NHS West Lincolnshire CCG
- offering people with mild frailty self-management support using the Age UK and NHS England co-produced Practical Guide to Healthy Ageing: NHS Bradford Districts CCG, NHS Calderdale CCG, NHS Hardwick CCG
- proactive care planning for people with severe frailty added to the GP Practice top 2% most at risk avoidable unplanned admissions (AUA) register: NHS West Lincolnshire CCG, NHS South Worchester CCG
Evidence based interventions for people with frailty: As a GP it would be useful to find out the frailty level of every patient I see in the consulting room. This would help inform my management. If the tool could also be linked to appropriate interventions then this would be even better and would act as a trigger for things to consider i.e. linked to a frailty template
Dr Lesley Freeman, GP & CCG Dementia Lead, NHS Leeds South & East CCG
The Future
Further development of the eFI is needed to increase its clinical utility – for example, a patient level eFI report will support sharing of an individual’s frailty index score or frailty diagnosis between primary care and community/secondary/tertiary care to enable targeting of evidence based interventions based on individual frailty needs.